Celiac Disease & Other Food Allergies: Celiac symptoms, lactose and gluten intolerance symptoms, gluten-free diet, and more
Celiac Disease & Other Food Allergies:
Celiac symptoms, lactose and gluten intolerance symptoms, gluten-free diet, and more

The only answer for those who experience the intestinal issues caused by celiac disease and gluten sensitivity: a gluten-free diet. The marketplace, fortunately, is enjoying more and more products to complement a wide variety of gluten-free recipes.
I. WHAT IS CELIAC DISEASE?
Celiac disease is a genetic autoimmune disorder that occurs when the body reacts abnormally to gluten, a protein found in wheat, rye, and barley. When people with celiac disease eat foods that contain gluten, an immune-mediated toxic reaction causes damage to their small intestine and also to other systems in the body. Celiac disease affects about 1 in 133 people, an estimated 3 million Americans. Approximately 85 percent of these are thought to be undiagnosed.
Specialists now confirm that another portion of the population is affected by non-celiac gluten sensitivity. Individuals with gluten sensitivity experience symptoms similar to celiac disease but without the autoimmune reaction or the intestinal damage.
Celiac disease is a lifelong condition that cannot be outgrown. It is often present without obvious symptoms. If left untreated by the gluten-free diet, it continues to cause (more or less “silently”) intestinal damage and can lead to the development of conditions such as osteoporosis, infertility and chronic anemia, as well as other related autoimmune disorders and even certain types of cancer.

Click the image to expand view. If you have celiac disease and accidentally eat gluten, your body mounts an immune response that attacks the small intestine. These attacks, as the Celiac Disease Foundation puts it, “lead to damage on the villi, small fingerlike projections that line the small intestine, that promote nutrient absorption. When the villi get damaged, nutrients cannot be absorbed properly into the body.”
Older Adults and Celiac Disease
Celiac disease was once considered a childhood condition that could be outgrown. Medical experts now know that celiac disease is a lifelong disorder that doesn’t occur just in childhood. New studies suggest it’s possible to develop celiac disease quite late in life. When researchers from Finland screened a large group of adults over age 55 for celiac disease in 2002 and then again in 2005, they detected several new cases during the three-year interval, indicating that the disorder can develop even in the elderly.
Similar results were reported in a study conducted in the United States by the University of Maryland Center for Celiac Research. The research revealed that as people in the study aged, the incidence of celiac disease increased.
Still unanswered is why a person would develop celiac disease at age 60, 70, 80, or even 90. There are theories on triggers, like changes in the intestinal bacteria, but these theories are not yet proven.
While younger patients are often able to heal quickly on a gluten-free diet, intestinal healing may take longer for older adults. The dramatic turnarounds in health sometimes seen after diagnosis and adherence to the gluten-free diet—feeling like a new person overnight—aren’t typical for those diagnosed at an older age. The intestines heal more quickly in those who are younger. Little children may heal in weeks or months while older adults may take years to recover and some may not ever get fully back to normal.
Celiac Triggers
As with all autoimmune diseases, celiac disease is thought to involve a complex interaction of genetic and environmental factors. Thus far, two genetic markers—HLA-DQ2 and HLA-DQ8—have been associated with the condition. Ninety-nine percent of those with celiac disease have one of these genetic markers. (Note that many people who don’t have celiac disease also have these markers.) Research is actively occurring to identify other genes that are also implicated in the onset of celiac disease and the list of genes is growing every year. It is thought, however, that their role is minor compared with the HLA-DQ2 and HLA-DQ8 markers.
Besides gluten, additional environmental factors may contribute to the onset of celiac disease. A particular event can activate, or “turn on,” the condition. Sometimes celiac disease is triggered—or becomes active for the first time—after stressful events, like surgery, pregnancy, childbirth, viral infection or severe emotional stress.
Infection may be a substantial trigger for celiac disease. Over the years, infections have been studied in connection with the onset of a variety of autoimmune conditions, including type 1 diabetes and rheumatoid arthritis.
When a report in the medical literature noted the symptomatic onset of celiac disease following a confirmed case of Campylobacter jejuni enteritis (traveler’s diarrhea), it was among the first to suggest that an environmental factor other than gluten—in this case, an infection—could be important to the onset of symptomatic celiac disease. A large, earlier study of children with genetic markers for celiac disease linked repeated rotavirus infections (one of the most common causes of childhood diarrhea) with an increased risk of developing celiac disease later in life.
More recently, it has become clear that the risk for developing celiac disease is increased by any type of recurring infections during early infancy.
Just how an infection might precipitate celiac disease or celiac symptoms is unclear, however. One theory is that repeated infections chronically stimulate the immune system, which may, in turn, trigger an autoimmune reaction in genetically susceptible people. Another theory is that a mechanism known as molecular mimicry is to blame. Here, a foreign protein, such as an infectious bacteria or virus, tricks the body into attacking its own cells.
First-degree relatives should have serological blood tests every three years or so, as normal results don’t exclude the possibility that celiac disease will develop later in life.
Should You Be Screened?
Anyone with celiac symptoms should be screened for the disease. Testing is also recommended for individuals at higher risk for celiac disease, even in the absence of symptoms. They include:
- First-degree relatives of patients with celiac disease
- Insulin-dependent diabetes mellitus (requiring insulin therapy)
- Graves disease
- Hashimoto’s thyroiditis
- Down syndrome
- Turner syndrome
- Williams syndrome
- Unexplained infertility or recurrent miscarriage
- Unexplained high transaminases
Antibody Testing
To diagnose celiac disease, doctors screen the blood for high levels of auto-antibodies—proteins that react against the body’s own cells or tissues.
The first step in diagnosing celiac disease is usually a blood test to measure levels of certain auto-antibodies produced by the immune system in response to ingested gluten. As a result, it’s important to be eating a regular, gluten-containing diet when tested for celiac disease; if you have been on the gluten-free diet longer than a couple of months, results may be negative even if celiac disease is present.
Doctors screen with a panel of blood tests, since each test alone can vary in terms of specificity and sensitivity. A positive blood test indicates that a person needs a biopsy of the small intestine; it is not a celiac diagnosis. Once diagnosed, these same blood tests can be used to help monitor improvement on the gluten-free diet.
- Genetic testing: When blood tests are unclear or when a patient is already on the gluten-free diet, a genetic test may help clarify the diagnosis—it rules out the likelihood of celiac disease when negative. Using a small sample of blood, cheek cells or saliva, the genetic test looks for two markers associated with celiac disease, HLA-DQ2 and HLA-DQ8.Human leukocyte antigens (HLA) are proteins, of which DQ is a subset, that are found on the surface of almost every cell in the body and are a key component of the immune system. While everyone has slightly different HLA proteins, each of us has two sets, one inherited from each parent.Ninety-nine percent of celiacs have one of these two genetic markers. Thus, a negative genetic test essentially rules out celiac disease. A positive test result, on the other hand, does not indicate the patient has or will develop celiac disease. In fact, up to 40 percent of the population has one of these markers and very few of these people will ever get celiac disease.
- Intestinal biopsy: The intestinal biopsy is still the gold standard for diagnosing celiac disease. If blood tests and symptoms suggest celiac disease, a biopsy of the small intestine is performed to confirm the diagnosis.During an upper endoscopy, a gastroenterologist eases a long, thin tube called an endoscope through the mouth and into the beginning of the small intestine.
- As the tube is making its way to the small intestine, a camera on the end sends a video image to a monitor so that the physician can visually assess any inflammation. Tissue samples from the small intestine are biopsied to check for damage to the villi, the fingerlike projections in the small intestine that absorb nutrients.The biopsy requires the patient be on a regular (gluten-containing) diet in order to be accurate. If taken alone, it may still miss the portion of the small intestine with flattened villi. In fact, because celiac disease doesn’t cause uniform intestinal damage, experts recommend that four to six different samples be taken from the second or third part of the duodenum. A biopsy may need to be repeated over time, since normal results don’t exclude the possibility the disease will develop later in life.
- Skin biopsy: A skin biopsy is the gold standard for diagnosing dermatitis herpetiformis (DH), an uncomfortable skin condition associated with celiac disease. It’s characterized by an itchy, blistering rash, often on the elbows and knees. The skin biopsy must be performed on uninvolved skin adjacent to the affected area since the inflammatory reaction interferes with immunological testing.
- Nutrient testing: Patients, especially adults, should be tested for nutritional deficiencies, because of the malabsorption associated with celiac disease. Vitamins and minerals are acquired through the diet and affect every system in the body in a complex interaction. Thus, nutrient testing is important to determine the condition of the body.When the digestive tract is damaged, as in celiac disease, the body is unable to properly absorb the foods consumed. Even with a healthy diet, the body is unable to fully extract the nutrients it requires.
- Follow-up testing: Although the symptoms of celiac disease vary from person to person, some basic tests should be part of every patient’s annual health checklist. Celiac specialists recommend both antibody and nutrient testing after diagnosis and certain tests yearly thereafter.
People with celiac disease are usually monitored annually. Those who were very sick prior to diagnosis should be seen more frequently.
Children generally respond more quickly than adults to the gluten-free diet but they also need time to heal. While antibody levels typically return to normal in 12 months, it occasionally takes longer. In part, the speed of normalization of the antibodies depends on how high they were to begin with; higher toiters require longer (often more than one year) to normalize. Thus, repeat testing in one to three months may only serve to raise parents’ anxiety.
After Diagnosis
After you have been officially diagnosed with celiac disease, make sure to consult with a doctor and nutritionist who specialize in celiac disease. If you’re not currently receiving specialized celiac care, consider seeking out the closest celiac research and treatment.
It’s a good idea to see a specialist for regular check-ups and follow-up blood tests to be certain you’re not inadvertently ingesting gluten. Celiacs are typically more susceptible to other medical conditions, ranging from lactose intolerance (usually transient) to other autoimmune disorders, and an alert doctor can work closely with you to lower the risks.
As an important aside, a specialist can counsel your relatives about whether they should undergo blood tests or genetic screening for this inherited autoimmune disorder. Your family members—particularly first-degree relatives—are at risk for contracting the disease. Undetected and untreated, celiac disease can wreak havoc on the immune system and set loved ones up for serious medical problems in the future.
II. SPECTRUM OF GLUTEN-RELATED DISORDERS
In recent years, it’s becoming increasingly clear that the reaction to gluten is manifested in more than just celiac disease. Other gluten-related disorders—such as dermatitis herpetiformis, gluten ataxia, and non-celiac gluten sensitivity—are part of a spectrum of gluten reactions.
At the 2011 Consensus Conference on Gluten Sensitivity in Oslo, a panel of 15 experts referred to these conditions as “gluten-related disorders” and proposed classifying them based on the type of immune reaction triggered by gluten: allergic, autoimmune, or possibly immune-mediated.
The immune system responds to gluten in different ways, depending on who you are and your genetic disposition. Different organs can be affected by different types of gluten sensitivity. In celiac disease, the small bowel is affected. In dermatitis herpetiformis, the skin is targeted, resulting in an itchy rash. Gluten ataxia impacts the brain; it’s a neurologic condition characterized by the loss of balance and coordination.
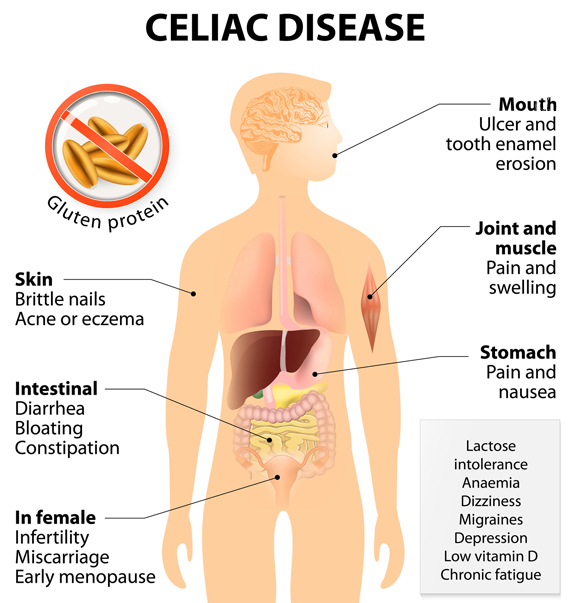
How does celiac disease affect us? As the chart here shows, it can wreak havoc on everything from the mouth to joint pain to intestinal and stomach issues to skin problems.
Depending on the person and their genetic makeup, one person may develop an autoimmune condition, such as celiac disease, dermatitis herpetiformis or gluten ataxia. The next person may develop non-celiac gluten sensitivity.
Spectrum Categories
The Oslo researchers divided the gluten-related spectrum into three main categories:
- Allergic. A wheat allergy occurs when the body produces antibodies (usually IgE) in response to wheat (including gluten, the protein found in wheat). These antibodies circulate throughout the bloodstream, triggering an immune response (an allergic reaction), which occurs within minutes or up to a few hours after gluten exposure.
- Autoimmune. This includes celiac disease, dermatitis herpetiformis, and gluten ataxia. In celiac disease, gluten sets off an autoimmune reaction that causes the destruction of the villi in the small intestine, interfering with the absorption of nutrients from food. Dermatitis herpetiformis is known as the skin form of celiac disease, characterized by a blistering, itchy rash. Gluten ataxia is characterized by damage to the cerebellum, resulting in difficulty with balance and coordination.
- Immune-mediated. This includes non-celiac gluten sensitivity. Non-celiac gluten sensitivity is a poorly understood entity thought to possibly have its own immune mechanisms affecting different parts of the body. Many people with non-celiac gluten sensitivity have celiac-like symptoms but have no corresponding damage to the gut. It is possible, but as yet unproven, that their immune reactions are related to involvement of the innate immune system, a primitive system that sets up barriers to repel invaders, rather than the adaptive immune system. The onset of symptoms is hours to days after gluten exposure. It must be stressed again that research is ongoing about non-celiac gluten sensitivity and that the condition remains ill defined at present.
Dermatitis Herpetiformis
Dermatitis herpetiformis (DH) is a skin rash that affects 15 to 25 percent of people with celiac disease. It is characterized by an intensely itchy, blistering rash that may occur anywhere on the body, including limbs, trunk, groin, hands, fingers, face, scalp, and along the hairline. The rash is bilateral in nature; both knees or both arms are usually affected, not just one.
Many people with DH have none of the outward digestive symptoms of celiac disease, and only about 40 percent of them have the positive blood tests for celiac disease. But they often have the same intestinal damage as those with celiac disease.
Gluten Ataxia
Gluten ataxia is a neurologic condition characterized by the loss of balance and coordination. However, it can also affect fingers, hands, arms, legs, speech and even eye movements. Typical symptoms include difficulty walking or walking with a wide gait, frequent falls, difficulty judging distances or position, visual disturbances and tremor.
With gluten ataxia, damage takes place in the cere?bellum, the balance center of the brain that controls coordination and complex movements like walking, speaking and swallowing. Purkinje cells in the cerebellum, key in maintaining balance, are thought to be lost in gluten ataxia.
Associated Complications
Infertility: When researchers at the Celiac Disease Center at Columbia University screened 188 women with unexplained infertility, almost 6 percent had celiac disease—a rate nearly six times higher than expected, making celiac disease an important association of unexplained infertility, according to a study published in The Journal of Reproductive Medicine in 2011.
Untreated celiac disease can rob a woman’s body of nutrients, but malnourishment isn’t the only mechanism behind infertility. Antibodies to tissue transglutaminase (tTG)—one of the key markers of celiac—can have an effect on the placenta’s development.
Osteoporosis: When celiac disease goes untreated, the small intestine is injured and can’t properly absorb nutrients, including calcium. Calcium is so critical for nerve and muscle functions—like heartbeat—that if it’s not absorbed from food, survival mechanisms take over and the body taps the bones for calcium. Over time, this leads to bone loss. Gluten can also increase the systemic level of inflammation in the body. Inflammation causes proteins, called cytokines, and other inflammatory mediators to circulate in the blood and interfere with bone growth.
Chromosomal disorders: Individuals with chromosomal abnormalities, such as Down syndrome, Turner syndrome, and Williams syndrome, have a predisposition toward autoimmune diseases (including celiac disease), endocrine disorders and cancers.
Neurological Disorders
Certain neurological disorders—idiopathic epilepsy (epilepsy without a known cause), ataxia (unstable gait, clumsiness), peripheral neuropathy (tingling or numbness in the hands or feet), schizophrenia and even recurrent headaches—can be associated with celiac diease. Some syndromes, like epilepsy with calcification in the brain, are definitely linked to celiac disease. In addition, certain psychiatric disturbances—hallucinations, depression, anxiety, suicide ideation—occur more frequently in patients with celiac disease.
Celiac disease can also present as autistic-like behaviors. Although autism and celiac disease are distinct, unrelated entities, some autistic-like behaviors are common in celiac disease, especially in young children. A child with undiagnosed celiac disease may, in fact, appear sad, introverted, unwilling to socialize or communicate even with his or her parents, or the child may be cranky and excessively irritable.
Neurologic, psychiatric, emotional, and autistic-like manifestations have been described in celiac patients who show minimal or no GI symptoms and no damage in the small intestine.
Fortunately, all these symptoms, including depression, anxiety and hallucinations, are likely to regress on a gluten-free diet.
Autoimmune Disease
Celiac disease is associated with an increase in autoimmune disorders. Studies have proven that the older a patient is upon being diagnosed with celiac disease, the greater his chances of developing other autoimmune disorders, like hypothyroidism but also, less commonly, hyperthyroidism, Addison’s disease, vitamin B12 deficiency, vitiligo (spotty loss of skin pigment), and alopecia (hair loss), among others.
Type 1 Diabetes
Celiac disease and type 1 diabetes are both chronic, lifelong autoimmune diseases. The two conditions have a genetic link, sharing some genes and environmental factors that may cause the immune system to attack the villi in the small intestine (in celiac disease) and beta cells in the pancreas (in type 1 diabetes). Researchers believe that celiac disease and diabetes have at least seven genes in common, and there may be more.
Other Autoimmune Diseases
Autoimmune disorders result when the body’s leukocytes (white blood cells)—which normally fight infection—attack and destroy healthy body tissue. Celiac disease is associated with an increased prevalence of other autoimmune conditions, including multiple sclerosis, Hashimoto’s thyroiditis (which results in hypothyroidism), Graves disease (which leads to hyperthyroidism), Addison’s disease, and autoimmune hepatitis.
III. NON-CELIAC GLUTEN SENSITIVITY
For years, many people reported having celiac-like symptoms—abdominal pain, fatigue, foggy mind, joint pain, tingling of the extremities, even depression—but they repeatedly tested negative for celiac disease and responded positively to the gluten-free diet. Now specialists recognize that these patients may have non-celiac gluten sensitivity, a condition that is distinct from celiac disease.
How Common Is Non-Celiac Gluten Sensitivity?
Studies have now demonstrated that non-celiac gluten sensitivity is a distinct medical condition that differs from celiac disease. Celiac disease is considered a subset of gluten sensitivity.
Anyone with celiac disease, by definition, is gluten-sensitive. However, not all gluten-sensitive people have celiac disease. Unlike celiac disease, non-celiac gluten sensitivity causes no measurable intestinal damage. Classic symptoms are gastrointestinal, such as diarrhea, bloating, or constipation. Some people report symptoms ranging from clumsiness, brain fog, and depression to ADHD or autistic-like behaviors.
Patients with non-celiac gluten sensitivity might have various reactions to gluten. In a study of 347 gluten-sensitive patients conducted by the University of Maryland, 68 percent experienced abdominal pain, 40 percent had eczema or a rash, and approximately a third reported headache, diarrhea, fatigue, or “foggy mind.” Depression, anemia, numbness in the legs, arms, or fingers, and joint pain were also frequently reported.
How Is It Diagnosed?
Currently, non-celiac gluten sensitivity is a diagnosis of exclusion; it’s diagnosed only after other conditions are ruled out. Non-celiac gluten sensitivity is not an allergic condition, is not an autoimmune reaction to gluten, does not cause any significant damage to the small intestine, and is not associated with HLA genes (as is celiac disease).
There are no genes that are currently known to be associated with non-celiac gluten sensitivity and there are no diagnostic markers, such as anti-gliadin antibodies, stool tests, saliva tests, or biopsy, for conclusively diagnosing the condition.
Non-celiac gluten sensitivity is typically determined by a positive response to the gluten-free diet. The defining element of non-celiac gluten sensitivity: Feeling better when you don’t eat gluten.
IV. THE GLUTEN-FREE DIET
Keeping a strict gluten-free diet—avoiding all foods that contain wheat, rye, or barley—is essential for those with celiac disease or non-celiac gluten sensitivity.
People on a gluten-free diet can eat a well-balanced menu with a wide variety of foods. Unprocessed meat, fish, rice, fruits, and vegetables do not contain gluten, plus there are plenty of gluten-free breads, pasta, and cookies that use rice flour and alternative grains. The key is to focus on what you can eat, not what you cannot.

The key to a gluten-free diet: Focus not on what you must avoid, but on what you can eat, from creative pasta salads to gluten-free breads and soups to creative pasta. And always, lots of fruits and vegetables.
Grains Allowed
- Amaranth
- Arrowroot
- Beans
- Buckwheat
- Corn (maize)
- Flax
- Garfava
- Millet
- Montina
- Nut flours
- Potato
- Quinoa
- Rice
- Sorghum
- Soy
- Tapioca
- Teff
The gluten-free diet requires a completely new approach to eating. People with celiac disease have to be extremely careful about what they buy for lunch at school or work, eat at cocktail parties, or order from restaurants.
Cheating (eating food containing gluten) or cross-contamination—even as small as one-eighth of a teaspoon—can cause intestinal damage. A dietitian who specializes in celiac disease can help patients learn about their new diet.
Grains Not Allowed in Any Form
- Wheat (einkorn, durum, faro, graham, kamut, semolina, spelt)
- Rye
- Barley
- Triticale
Gluten-Free Basics
A strict gluten-free diet—one free of all forms of wheat, barley, and rye—is necessary to help prevent both short-term and long-term consequences of celiac disease. Even miniscule amounts of gluten—a crumb on a shared stick of butter—can be enough to cause problems for those with celiac disease.
Don’t eat a food if you are unable to verify the ingredients or if the ingredient list is unavailable. Regardless of the amount eaten, if you have celiac disease, damage to the small intestine occurs every time gluten is consumed, whether symptoms are present or not.
Understanding these dietary requirements (see “Grains Allowed” and “Grains Not Allowed in Any Form” sidebars) will enable the newly diagnosed to read labels of food products and determine if a product is gluten free.
Foods/Products That May Contain Gluten
- Beers, ales, lager
- Breading and ?coating mixes
- Brown rice syrup
- Communion wafers
- Croutons
- Dressings
- Drugs and over-the-counter medications
- Energy bars
- Flour and cereal products
- Herbal supplements
- Imitation bacon
- Imitation seafood
- Marinades
- Nutritional supplements
- Oats
- Pastas
- Processed luncheon meats
- Sauces, gravies
- Self-basting poultry
- Soup bases
- Soy sauce or ?soy sauce solids
- Stuffings, dressings
- Supplements
- Thickeners (roux)
- Vitamins & minerals
Pantry Preparation and Kitchen Cleanliness
It’s essential to prevent gluten cross-contamination, as even a tiny bit of gluten can cause health problems for people with celiac disease. Clean or replace the items in your kitchen where gluten contamination can occur—scratched pans, the toaster, colanders, cutting boards, your food mill, and other objects. Scrub your counters and put utensils, pans, bowls, cutting boards, and sponges in the dishwasher before baking gluten-free.
Do your homework to truly understand cross-contamination, gluten-containing ingredients, and food labeling so that your kitchen becomes a safe haven, one that you can rely on for tasty, uncontaminated foods. If your kitchen is not fully gluten-free, take steps to make sure there is no cross-contact with gluten before baking. Be aware that particles of wheat flour can linger in the air for 24 to 36 hours.
If someone in your household plans to continue to eat gluten, organize your pantry and cabinets so that no gluten-containing foods, pots, or pans are mistakenly used. Use clear plastic bins in your pantry to segregate items so there are no mix-ups when unpacking the groceries or when reaching for cereals or snacks. Color-code pots, pans, utensils, and the like with fun-colored duct tape so that it’s easy to tell which are dedicated for gluten-free use.
Take out everything in the pantry, refrigerator, and freezer and check their labels. Keep a permanent marker in the kitchen and write “GF” (gluten-free) on all safe foods and condiments. Use separate jars of mustard, peanut butter, and jelly and separate sticks of butter to avoid cross-contamination from wheat crumbs. Or buy squeeze bottles for condiments, which reduces the chance of cross-contamination. Don’t buy foods from bulk bins that are prone to contamination from other grains.
Buy some prepared gluten-free foods, too: frozen pizza, pasta, soup, pretzels, and other favorite snacks—whatever you enjoyed eating before adopting the gluten free diet. Having these items on hand will keep you from feeling deprived and help you avoid the temptation to eat gluten. Try a few different brands to figure out which you like best. The best ways to find tasty alternatives are to get connected with others by joining a support group and to attend gluten-free fairs and expos, where you can sample different items before buying.
You’ll also want to stock some gluten-free baking mixes and a reliable all-purpose gluten-free flour blend. Find an all-purpose flour blend that can be used for almost everything from fish sticks and tempura to birthday cake and sandwich bread. Once you’ve gained confidence, you can then experiment with the growing variety of tasty alternative gluten-free flours made from whole grains and seeds. These offer rich flavor, nutrients, and fiber that will enhance your culinary repertoire.
Even if you’ve never baked from scratch, consider doing it now. Despite all the new gluten-free products available, many just don’t taste like the foods you remember. That’s where you and your oven come in. By taking a proactive approach to baking, and you’ll be able to enjoy, once again, any item you enjoyed prior to your diagnosis. Bread, cookies, cake, muffins, pizza—you’re limited only by your imagination.
Labeling Lingo
The sweeping legislation known as FALCPA, the Food Allergen Labeling and Consumer Protection Act of 2004, requires clear labeling of the so-called top 8 allergens (milk, eggs, tree nuts, peanuts, fish, shellfish, soy, and wheat). Thus, all food containing wheat must declare it on the label.
In August of 2013, the term “gluten-free” received an official definition. That’s when the U.S. Food and Drug Administration (FDA) issued a regulation for all “gluten-free” references on food labeling. “The definition provided consumers—especially those with celiac disease—the assurance that ‘gluten-free’ claims on food products will be consistent and reliable across the food industry,” according to a release at FDA.gov, “and gave them a standardized tool for managing their health and dietary intake.
“FDA’s regulation for gluten-free food labeling standardized what ‘gluten-free’ means on the food label,” the release continues. “‘Gluten-free’ is a voluntary claim that manufacturers may elect to use in the labeling of their foods. However, manufacturers that label their foods ‘gluten-free’ are accountable for using the claim in a truthful and not misleading manner, and for complying with all requirements established by the regulation and enforced by FDA.”

The FDA keeps a close watch on food products claiming to be gluten-free. You’ll see a variety of different labels on products; make sure you look at the ingredients to be sure an item backs up its claims (see “Labeling Lingo” section).
The FDA’s regulation means that a gluten-free label indicates a food doesn’t contain:
- 20 ppm or more of gluten.
- Any ingredient that is a prohibited grain, such as wheat, barley, rye, or their derivatives.
- Any ingredient derived from a prohibited grain that has not been processed to remove gluten, such as barley malt extract or malt vinegar.
- Any ingredient derived from a prohibited grain that has been processed to remove gluten if 20 ppm or more gluten remains in the food, such as wheat starch or modified food starch.
- Foods inherently free of gluten must indicate as much, such as “milk, a gluten-free food,” or “all milk is gluten free.”
Oats must contain less than 20 ppm of gluten to bear a gluten-free claim. In addition, a claim cannot suggest all foods made from oats are gluten free.
Permissible synonyms for “gluten free” include “free of gluten,” “without gluten,” and “no gluten.”
Gluten-Free Flour Power
With these alternative flours, you can continue making your favorite foods without compromising taste and texture. In fact, you can add essential vitamins, minerals, protein and fiber to your baked goods, fortifying your diet in flavorful ways. From beans and grains to tubers and seeds, there’s a rich and wonderful array of delicious and nutritious flours waiting for you.
- Beans and Legumes
- Bean flours: Varieties include chickpea (garbanzo), bean (navy, pinto and red) and soy. Garfava flour is a blend of flours made from garbanzo, fava beans and Romano beans. High in protein, fiber and calcium, these flours work best with heavier foods, such as breads and spice cakes.
- Pea flour and green pea flour: Both have benefits similar to bean flours but without the strong aftertaste. High protein content adds structure to baked goods without any distinct flavor.
- Grains
- Amaranth: An ancient food used by the Aztecs, the seeds of the broad-leafed amaranth plant are milled into flour or puffed into kernels for breakfast cereals. High in protein, calcium and iron, this mildly nutty-tasting flour adds structure to gluten-free baked goods and helps them brown more quickly.
- Corn flour: Milled from corn kernels, this is finely ground cornmeal that comes in yellow and white varieties. One form of corn flour is masa harina (milled from hominy) used in making corn tortillas. If corn flour isn’t available, you can make your own by grinding cornmeal into a fine powder in a food processor. High in fiber with a slightly nutty taste, corn flour is a good source of fiber, riboflavin, niacin, folate, iron and thiamin.
- Cornstarch: A flavorless white powder that lightens baked goods to make them more airy. Cornstarch is highly refined and has little nutritive value. Store in a sealed container in a dry location.
- Cornmeal: With a larger particle size than corn flour, cornmeal lends excellent texture to foods and has a nutty and slightly sweet taste. Cornmeal comes in yellow and white varieties and in fine, medium and coarse grinds. Select finer grinds for baking and for polenta. Use coarse meal for breading. High in fiber, iron, thiamin, niacin, B-6, magnesium, phosphorus and potassium.
- Millet: An ancient food, possibly the first cereal grain used for domestic purposes, millet imparts a light beige or yellow color to foods. Millet is easy to digest, and its flour creates light baked goods with a distinctive mildly sweet, nut-like flavor. High in protein and fiber and rich in nutrients, millet adds structure to gluten-free baked items.
- Oat flour and oats: High in fiber, protein and nutrition, pure, uncontaminated gluten-free oats add taste, texture and structure to cookies, breads and other baked goods. If oat flour is not available, you can make it by grinding oats in a clean coffee grinder or food processor. (Quinoa flakes can be substituted for whole oats in most recipes.) Store in a tightly sealed container in a cool, dry place or freeze to extend the shelf life.
- Rice flour: This is the gluten-free flour that’s used most often. It’s available as brown rice (higher in fiber), sweet rice (short grain with a higher starch content) and white rice. Rice flour is easy to digest and blend. The texture varies depending on how it’s milled—fine, medium or coarse. Fine grind is used for cookies, biscotti and other delicate baked goods. Medium grind, the most readily available, is suitable for most other baking. Coarsely ground is best for cereal and coatings. White rice flour has a bland taste. Brown rice is slight nutty.
- Sorghum flour: Some believe this flour, also called milo or jowar flour, tastes similar to wheat. Available in red and white varieties, it has a slightly sweet taste and imparts a whole-wheat appearance to baked goods. Sorghum is high in protein, imparting all-important structure to gluten-free baked goods. It’s also high in fiber, phosphorous, potassium, B vitamins and protein.
- Teff flour: Milled from one of the world’s smallest grains, teff is a key source of nutrition in Ethiopia. It’s available in dark and light varieties. High in protein, fiber and calcium, teff imparts a mild, nutty taste to cookies, cakes, quick breads, pancakes and waffles.
- Grasses
- Buckwheat: Despite its name, buckwheat is not a wheat. Instead, it is a fruit from the Polygonaceae family, which also includes rhubarb and sorrel. Buckwheat has a strong, robust flavor that combines well with other gluten-free flours. A great source of protein and eight essential amino acids, this flour is high in fiber and B vitamins. It’s available in light, medium and dark varieties; light buckwheat flour is usually preferred for baking.
- Wild rice flour: This flour is not made from rice. It’s a wild aquatic grass originally grown in lakes, particularly in the Minnesota area. Wild rice is now grown in man-made paddies and, therefore, it’s more plentiful. Rich in folate, wild rice has a long shelf life because it is dried and slightly fermented. This flour’s very dark brown to black color adds a rich hue to pastries and other baked items. It has a hearty, interesting flavor and texture.
- Nuts and Coconut
- Almond flour and almond meal: Make your own almond flour by finely grinding blanched nuts in a clean coffee grinder. Don’t overgrind; almond flour can turn into almond butter very quickly. Leaving the skin on the almonds will darken the final baked product. Almond flour im?parts a sweet, nutty flavor to baked goods. High in protein, fiber, vitamin E and healthy fat, almond flour adds structure and texture to cakes, cookies and cupcakes. It can be substituted for oats in oatmeal cookies for people who cannot eat oats.
- Chestnut flour: Made from ground chestnuts, this flour imparts a nutty, earthy flavor to baked goods. High in fiber and low in protein, it is used widely by Italian bakers and cooks in everything from pasta (tagliatelle and gnocchi) to cakes, pancakes, breads, and muffins. Store in an airtight container at room temperature.
- Coconut flour: A low-carb, high-fiber flour with the subtle, sweet fragrance of coconut. It’s usually well tolerated by people who have multiple allergies. People on low-carb diets often bake with 100 percent coconut flour
- Seeds
-
- Flaxseed meal: This tiny but mighty seed is high in fiber and omega-3 fatty acids. Make your own flax meal by grinding flax seeds in a clean coffee grinder. (Whole flax seeds are not digestible.)

Flaxseed provides a boost of nutritional advantages—from fiber to omega-3 fatty acids to protein—for those on a gluten-free diet.
- Chia: Also called salba, chia seeds come from the Salvia hispanica plant. Hundreds of years ago, Aztec warriors would tie a bag of these seeds to their belts to sustain them during their conquests. The seeds were so important in Aztec culture that they were used as money. Considered a super food due to high levels of multiple nutrients and protein, chia is flavorless.
- Hemp flour: This protein-rich whole-grain flour imparts a nutty flavor to breads, muffins, cookies and ?pancakes. It is an excellent source of protein, containing all essential amino acids, and is very high in dietary fiber.
- Quinoa: Milled from a grain that’s native to the Andes Mountains, quinoa has a delicate, nutty flavor that’s similar to wild rice. This flour is easy to digest. Quinoa contains high levels of calcium, protein, complex carbohydrates, phosphorous, iron, fiber and B vitamins.
-
- Tubers
- Potato flour: Made from dehydrated potatoes, this fine yellow-white powder is high in fiber and protein.
- Potato starch: Made from the starch of dehydrated potatoes, this white powder is often used as a one-for-one substitution for cornstarch in recipes. It has excellent baking qualities, particularly when combined with eggs. Contains no protein or fat.
- Root flours (tapioca, arrowroot and sweet potato): Made from root plants, these flours are usually well tolerated by food-allergic people, even those with multiple allergies. High nutritional properties enhance baking performance and give baked goods a chewy texture and increased browning capabilities. Arrowroot flour is pleasant-tasting and versatile, good for making breads and bagels. Sweet potato flour, which has a yellow-orange hue, imparts its color to baked goods and has a taste that complements recipes containing chocolate, molasses, spices and such.
- Wine Flours
Wine flours (also called grape seed and grape skin flours) are produced from the byproducts of wine-making. Wine flours, which include chardonnay, merlot, cabernet sauvignon and riesling flours, contain the health benefits of wine, including omega-3 and 6 fatty acids, vitamin A, iron, and potassium, and they add color and subtle taste to recipes.
- Cabernet flour, the darkest and headiest of the wine flours, is good for making breads and lends a hint of molasses taste when used to thicken sauces.
- Merlot flour adds a taste punch to chocolate cake and a rich hue to sauces, especially those served with meats.
- Chardonnay flour has a buttery taste and gives a subtle graham-cracker flavor to baked goods.
- Reisling flour, slightly sweet, perks up the taste of breads and pasta; its flavor is ideal in desserts like cream puffs, pound cake, and cookies.
V. DINING OUT AND TRAVELING, GLUTEN-FREE
Once you’ve got a firm handle on eating gluten-free at home, you may be ready to broach an even broader subject: dining out at restaurants gluten-free, whether locally or when you’re traveling.
Finding Safe Options
Many restaurants now offer gluten-free menus and gluten-free options. However, it’s extremely important to be very careful and very clear when you order gluten-free food at a restaurant. While it is possible to have great gluten-free meals without incident, you must be careful and very specific to avoid any mishaps in food preparation or cross-contamination.

Having a night out at a restaurant doesn’t need to be a disaster for those who require a gluten-free diet. Just plan ahead; among the important considerations: Make a call to your destination restaurant and ask the questions posed here under “Preparing in Advance.”
Look for restaurants certified by the Gluten-Free Restaurant Awareness Program (GFRAP), operated by the Gluten Intolerance Group of North America (GIG).
- About 1,600 independently owned restaurants in the United States, Canada, and Germany have been GFRAP-certified as safe for gluten-free guests. Restaurants are listed on the GFRAP website, glutenfreerestaurants.org, by location and style of food.
- NFCA’s Gluten-Free Resource Education and Awareness Training (GREAT) Kitchens, celiaccentral.org/kitchens, equips chefs, restaurants and cafeterias with the knowledge and tools to safely provide customers with gluten-free meal options.
Look over restaurant websites to see whether they post gluten-free menus. Some establishments, especially restaurant chains, list specific ingredients and allergen information on their websites. When ordering from a gluten-free menu, inform the restaurant staff about the severity of your celiac disease and the need to prepare food without any cross-contamination.
Preparing in Advance
Call the restaurant during non-peak hours to inform them of your special dietary needs. Ask to speak with a chef or manager. If a manager isn’t available, ask for the manager’s name and the best time to call back.
Use a clear, confident, assertive style of communication. Ask questions until you’re satisfied. Here are a few suggestions:
- Can you accommodate a gluten-free diet? If the staff says yes, provide them with more information about what foods you cannot eat. Make sure they are aware of this and that they understand the severity of your reaction to gluten.
- Do you have a food allergy policy? If so, this is good news. Ask what company provided the training. The Gluten Intolerance Group, for example, offers restaurant training and certification through its GFRAP program.
- Do you have a designated area to prepare foods for special diets? Verify cooking procedures to check for cross-contamination. Ask about separate cutting boards and utensils. If restaurant staff don’t understand why they should keep food segregated during the preparation and cooking process, they don’t understand gluten-free cooking.
- Do you have specialty gluten-free products? When a restaurant carries prepared pancake mixes, gluten-free rolls or desserts from reputable manufacturers, it is taking gluten-free customers seriously.
- May I look at ingredient labels? If the restaurant is willing to show you ingredient labels, it’s a good sign they will accommodate your gluten-free diet.
At the Restaurant
The best time to dine at any restaurant is during the first hour of a service period. The staff is more alert and attentive and the kitchen is much cleaner. At off-peak hours, the kitchen is not as rushed.
The most important strategy when dining out is good communication. Again, be clear about your needs as well as the possible consequences. Assertive communication is the key to interacting with servers, managers, and chefs. Explain your gluten-free request and the possible consequences as well as the risks of cross-contamination. A calm, clear, and confident approach is the most effective way to ensure your needs are met.
If you’re part of a group, consider ordering last. Ordering last means you get the server’s full attention, you won’t feel pressured, and you won’t disrupt the table conversation. The person taking your order should write it down.
Select simple dishes with fewer ingredients; this goes for desserts, too. Avoid casseroles, sauces, gravies, soups, and marinades. A sautéed or baked item will minimize the use of common cooking equipment and shared utensils. Go through the list of ingredients, including garnishes, to make sure there is no hidden gluten.
Gluten-Free Travel
The thought of traveling can be daunting for people with celiac disease. Anxiety about meal planning and being away from the safety of home kitchens can often deter people from hopping in the car or boarding a plane and exploring a new city. If you’re afraid to risk an adventure outside your neighborhood, it’s time to push past the fear and venture forth. Safe, gluten-free traveling is very doable and highly rewarding. All it takes is a little extra planning and effort. The good news is that more places around the United States and internationally are accommodating gluten-free travelers.
Before you leave home, do your homework. Map out your trip in terms of allergy-friendly places to explore and safe restaurants to enjoy. Once you arrive, double-check your information, as menus can change. Locate natural food stores at your destination in advance, so you know where to purchase food throughout your trip.
According to market research sponsored by AllergyFree Passport and GlutenFree Passport, almost half of allergen-free and gluten-free consumers travel frequently, either within their own country or internationally. At the same time, more than 50 percent of resorts, spas, airlines, restaurants, and other hospitality professionals report a growing number of special-diet requests from their customers worldwide.
Regardless of destination, more than 85 percent of food-sensitive consumers are primarily concerned about two things when traveling: eating out safely in restaurants and the availability of special dietary snacks and meals. Airlines, accommodations, reactions to foods, and foreign languages are significant concerns for almost 50 percent of special-diet travelers.
How do you increase your personal comfort with traveling and reduce your worry? Educate yourself about your travel and eating-out options. Prepare yourself with snacks, medications, and back-up plans in the event of a mistake or emergency. Communicate your special dietary requirements effectively with airlines, hotels, cruise lines, restaurants, and hospitality professionals, as needed.
Yes, there are challenges with special-diet traveling, but food concerns needn’t keep you at home. Education, preparation, and communication are your keys to a safe journey, whether it’s around the corner, around the country, or around the world.
At the Airport
It’s essential to be prepared when traveling by air. Unfortunately, air travel often brings long delays. You may be stuck (and hungry) on a plane, in an airport, or at your destination. Pack nutritious bars and other healthy gluten-free snacks in a carry-on bag to eat during your flight. Bring enough for at least one meal, just in case your plane is delayed or plans change.
Make sure your snacks are allowed based on defined regulations. In the United States, the Transportation Security Administration (TSA) has strict standards on items that can be in your carry-on luggage. Visit tsa.gov/traveler-information for up-to-date information. Liquids (3 ounces or less) must be packed in one resealable, quart-size plastic bag per traveler. Be aware that certain foods, such as yogurt, salad dressing, or creamy dips, might be considered liquid and might be confiscated. Don’t bring cooling packs, as they typically contain chemical liquids or gels and will not make it through security. Instead, fill your resealable baggie or travel cooler with ice after you go through security, either at a food stand or on the plane.
Before you leave for the airport, use the Internet to investigate airport dining options in case you have an extended layover. Some airports, such as Boston, New York, Philadelphia, and Tucson, have food stands that carry gluten-free snacks (example: Cibo Express Gourmet Markets).
Once in the air, different types of special meals are offered based on flight duration, destination, and meal availability. Many airlines no longer offer much in the way of full meal service. Some airlines may offer snack boxes, which can be purchased during the flight; these pre-packaged items may not provide gluten-free foods. Be prepared by bringing your own safe snacks. To determine what foods are served or sold on board, review the airline’s website or call customer service before you book your flight.
On the Road
Take some simple steps to ensure safe eating while staying in hotels, resorts, bed & breakfasts, and condominiums. Start by contacting customer service at your place of lodging to address any questions and inform the representative about your gluten-free concerns before booking your reservations.
If you’re staying at an all-inclusive resort with a defined meal plan, discuss food alternatives with the appropriate culinary specialists and order your gluten-free meals in advance. If possible, obtain a mutually agreed-upon meal plan in writing. Three to five days before departure, confirm your special meal plan. Upon arrival, communicate your dietary concerns to the staff and provide feedback, as appropriate.
When booking accommodations, look for lodgings with microwaves, refrigerators, or kitchenettes so you can keep breakfast items and snacks in your room. Controlling at least one meal a day makes cross-contamination less likely. An all-suite hotel or executive-stay hotel is likely to have a kitchenette. In some hotels, you can request a mini-refrigerator for free or a small additional charge. Research local grocery stores and supermarkets located near the hotel so you can pick up food or have it delivered. Consider having your favorite online store ship products to the hotel during your stay.
Stock up on safe, healthy foods (visit a natural food store or farmer’s market) for a quick breakfast or late-night snack in your room. Gluten-free cereal, milk, and fruit provide for inexpensive, safe breakfasts that will save you time and money. Pack lunches to eat on the go. Always carry gluten-free snacks with you so you have a stash of safe food when sightseeing.
For road trips, buy an inexpensive cooler to keep in your rental car. Also, use your smart phone and the Internet as you’re traveling to map out local restaurant options and nearby grocery stores.
On a Cruise
More cruise lines are catering to guests with special dietary needs. Carnival, Celebrity, Crystal, and Princess Cruise Lines specify on their websites that gluten-free meals are available for their customers. In addition, Royal Caribbean and Disney Cruise Lines indicate that they can accommodate gluten-free guests.
Discuss meal alternatives with the chef or ship’s culinary specialist and order your gluten-free meals in advance. Determine whether designated wait staff will serve all meals to you throughout the cruise. Three to five days before your cruise, confirm your meal plan. Once you board the ship, meet with the dining room manager, designated server, wait staff, cabin crew, and/or chef to clarify and communicate your needs.
International Travel
It’s important to carry a dining card in the language of the country you’re visiting that contains an explanation of how you can be safely served. Be certain your translation is correct; a less-than-accurate translation will cause confusion and may be risky.
Read ethnic cookbooks as a guide for safer eating when traveling overseas. These recipes will give you an education in what questions to ask and what foods to order in restaurants. In particular, look at marinades and sauces, a source of hidden gluten in every country.
Focus on places and activities, not dining. You don’t have to indulge in five-star luxurious dining to have a great time. Make learning experiences and fun adventures the goal of your trip. Scale back on eating expectations—think basics, like being safe and eating healthy.
Preparation and packing are more extensive and important when you travel with special dietary needs—but do not let fear of gluten contamination keep you from leaving home. Pack gluten-free snacks to stave off hunger.
VI. LACTOSE INTOLERANCE VS. MILK ALLERGY
Lactose intolerance means you have difficulty digesting the sugar in milk. Milk allergy, often confused with lactose intolerance, is far more serious and involves an overreaction by the immune system on the protein in milk.
What’s the difference between lactose intolerance? A milk allergy, experts say, involves an attack on milk protein by the immune system, the part of the body that fights infections. In most cases, a type of antibody known as IgE (immunoglobulin E) responds to the presence of milk protein as if it’s a threat, or an invader. The result: immune responses that causes potentially dangerous symptoms.
Milk intolerance—often called lactose intolerance—refers to difficulty digesting the sugar found in milk. The sugar in milk is called lactose; lactase is the enzyme that digests it. Lactose intolerance is different than an allergy in that it refers to problems in the digestive system that stem from the missing enzyme lactase.
A milk allergy most often develops in people when they’re around a year old; by the time they’re 5 or 6, they typically outgrow the allergy. Around 10 to 20 percent will keep it their entire lifetime.
As for lactose intolerance, infants and young children usually have sufficient amounts of the lactase enzyme to digest milk sugars. The amount of lactase produced by the body, however, decreases over time. Thus, dairy intolerance more commonly develops in later childhood and adulthood. After onset, it’s less likely to resolve itself and requires diet changes.
Symptoms to Expect
If you have an allergic reaction to milk, you may feel it in multiple body systems affecting the skin, lungs, digestive system, and circulatory system. Symptoms can include itchy rashes, hives swelling (often of lips and face), wheezing and/or trouble breathing, and throat tightness. Vomiting, diarrhea, and abdominal pain are other symptoms, as are confusion, fainting, weakness, and low blood pressure.
A very small amount of milk can potentially trigger a reaction one or more of those reactions. Allergic symptoms usually begin minutes to an hour after ingestion. As a result, those with a milk allergy typically need to avoid milk completely.
And what about lactose intolerance? Symptoms usually involve only gastrointestinal issues, among them abdominal bloating or cramping, gas, vomiting, or diarrhea. If you’re lactose-intolerant, you may be able to eat small amounts of milk without a problem. Symptoms can occur up to several hours after ingesting dairy.



 What Are Sulfites and Are They Bad for You?
What Are Sulfites and Are They Bad for You?  Sesame Allergy: The 9th Most Common Food Allergy
Sesame Allergy: The 9th Most Common Food Allergy  Lupin Allergy: Are You At Risk?
Lupin Allergy: Are You At Risk? 