Diabetic Neuropathy: What It Means, How to Treat It
Diabetic neuropathy is a term used to describe damage to nerves in the body caused by prolonged exposure to high blood glucose levels in people with diabetes.
Diabetic neuropathy is a relatively common complication of diabetes. Some 60 to 70 percent of all people with diabetes experience some form of neuropathy in their lifetime.
While the reason this happens isn’t fully understood, researchers think that blood glucose affects how nerves transmit signals in the body and also damages the walls of blood vessels that supply those nerves.
Who Is at Risk for Diabetic Neuropathy?
Diabetic neuropathy can occur in anyone with diabetes, whether it’s type 1 or type 2, but there are certain risk factors that increase your odds of developing it:
- Duration of diabetes: The longer you have had diabetes, the more likely it is that you may develop diabetic neuropathy.
- High blood glucose: Poorly controlled blood glucose levels, particularly over a prolonged period of time, increases the risk of developing diabetic neuropathy.
- Obesity: Being obese or carrying excess weight is a risk factor for diabetic neuropathy
- Smoking and alcohol: Smoking and excessive alcohol consumption can lead to nerve damage and increase the risk of diabetic neuropathy.
- Genes: Some people appear to be genetically more susceptible than others to nerve disease whether or not they have diabetes.
- Autoimmune factors: Some individuals have inflammation of their nerves caused by an autoimmune response which increases their risk of diabetic neuropathy.
What Are the Types of Diabetic Neuropathy?
There are four main categories of diabetic neuropathy some of which can be called by different names:
- Peripheral Neuropathy: This is the most common form of diabetic neuropathy. It typically affects the nerves of the legs and feet followed by the arms and hands causing any of a number of symptoms including numbness, pain, tingling, weakness, loss of feeling, sensitivity to touch, and loss of reflexes.
- Autonomic Neuropathy: Autonomic nerves control involuntary functions in the body ranging from blood pressure to urination to digestion. Any of the nerves that are part of the autonomic nervous system can be damaged in autonomic neuropathy leading to problems including: urinary retention or incontinence, erectile dysfunction, constipation or diarrhea, difficulty swallowing or delayed gastric emptying, body temperature dysregulation, blood pressure and/or heart rate dysregulation, vaginal dryness, and inability to detect symptoms of low blood sugar or hypoglycemia.
- Proximal Neuropathy: This is sometimes called radiculoplexus neuropathy or diabetic amyotrophy and affects the nerves of the thighs, hips, or buttocks. It is more common among older individuals and those with type 2 diabetes. People suffering from proximal neuropathy may experience pain, weakness, and eventually muscle loss in the thighs, hips, and/or buttocks which can spread to the legs. It often affects one side of the body but can affect both. Some people may not be able to go from a sitting to standing position without assistance.
- Focal Neuropathy: This neuropathy, also called mononeuropathy, is sudden in onset and typically affects one specific nerve but is usually a short-term problem (lasting only weeks to months) with no long-term damage. The symptoms and signs depend on the nerve affected but examples include problems with focusing the eye, temporary paralysis of facial muscles, pain in the front of the thigh or outside of shin, chest pain that may be mistaken for a heart attack, and abdominal pain that may be mistaken for appendicitis.
Diagnosis of Diabetic Neuropathy
Diabetic neuropathy is most often diagnosed by a history of symptoms and physical exam. Your doctor will perform a neurologic exam which includes among other tests, checking reflexes, vibration and touch sensitivity, and muscle strength.
Your physician also will check your heart rate and blood pressure and assess how they are affected when you change positions. In addition, your doctor may choose to order one or more tests including nerve conduction studies and electromyography (EMG).
Treatment Options for Diabetic Neuropathy
The first steps in treating diabetic neuropathy involve improving your overall diabetes management through tighter blood glucose control, healthy eating, exercise, smoking cessation, and blood pressure control—all of which help to prevent further nerve damage. Your healthcare provider may also provide treatment options directed towards the specific problem you are experiencing as a consequence of neuropathy such as medication to speed digestion or medication for erectile dysfunction.
For general pain relief in diabetic neuropathy, some people experience relief from anti-seizure medications (such as gabapentin and pregabalin) and anti-depressants (such as desipramine and duloxetine). These medications have side effects, however, so you and your healthcare provider will need to discuss the whether the potential benefits of using them outweigh the risk of those side effects.
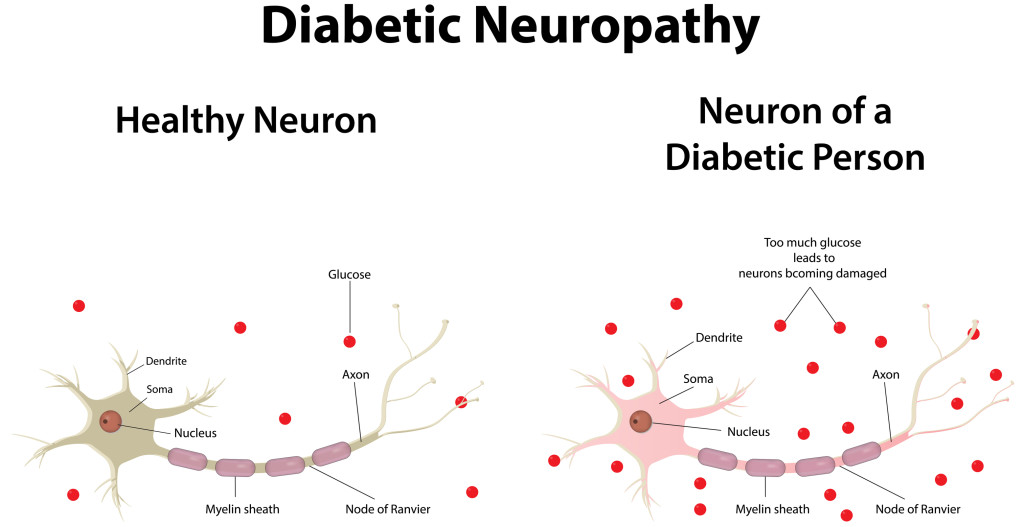
Healthy neuron, left, and neuron of a diabetic person, right, with the nerve’s myelin sheath compromised.
Originally posted in 2016, this post is regularly updated.


 Savor the Sweet Potato
Savor the Sweet Potato  Type 3 Diabetes: Does Diabetes Cause Memory Loss?
Type 3 Diabetes: Does Diabetes Cause Memory Loss?  Review These Blood Donation Requirements Before Giving Blood
Review These Blood Donation Requirements Before Giving Blood 
Neuropathy in the lower extremities is one consequence of diabetes. Neuropathy refers to any diseased condition of the nervous system.
© Flashon Studio | Dreamstime.com